As an athlete, there is nothing worse than getting injured during warm-up. It’s one thing to get tackled during a match…but getting injured trying to change direction seems a little ridiculous. Well, many years ago that was my meniscus. Then, I didn’t know much about meniscus injuries, but I’m glad I choose physical therapy. No surgery completed and still after many years, I am able to participate in activities without knee pain. So, if you have an injured meniscus, listen up and learn why physical therapy should be your 1st option, whenever possible!
What is a meniscus?
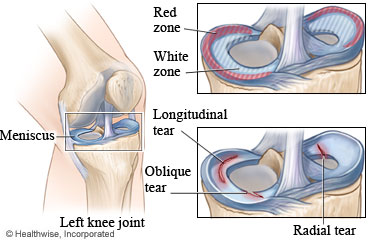
- It is a cartilage located between your femur (thigh bone) and tibia (shinbone)
- Composed of connective tissue and collagen that’s essential for providing strength and cushion across the knee during weight-bearing activities.
- Other functions:
- Serves as secondary stabilizers, ensures smooth movement of the joint, helps prevent hyperextension of knee and protects the joint space
- Other functions:
- Medial menisci
- Crescent-shaped with many attachments to structures around the knee, limiting its mobility
- Lateral menisci
- Circular, smaller and more mobile than the medial menisci
***Why is there a high incidence of injury to medial vs lateral menisci?***
ANSWER: As noted, the medial menisci has several attachments (resulting in less mobility) and also has attachments along the tibia which contributes to stability, making it more susceptible to injury.
Mechanism of Injury
- A combination of loading and rotational forces can result in a shear load on your mensicus
- When your knee is straight, there’s approximately 40-60% of load acting on the knee joint. As you bend your knee, your load increases on the meniscus. Makes complete sense why turning pivoting can result in an injury!
Healing time frame
- Varies for each individual: dependent on various factors: previous knee history, extent of meniscus injury, location, etc.
- Location
- While the meniscus has blood supply on the outer rim (red zone), there is limited blood supply on the inside (white – white zone) which contributes to the healing time frame (See picture above).
- ***Realize, one may not necessarily have symptoms, as some tears occur between the collagen, not affecting the biomechanics of the knee.
**How long will it take my meniscus to heal?**
ANSWER: The general tissue healing time frame for connective tissue is 4-8 weeks. It all depends on the complexity of the tear and location. A small tear, localized to the peripheral (outer) third where sufficient blood supply offers a better chance of healing.
Risk factors of meniscus injury
- Cutting and pivoting sports (soccer and rugby)
- Female sex
- Older age
- Higher body mass index (BMI)
- Lower physical activity
- Delayed ACL reconstruction
- Occupation requiring repetitive movement: squatting, kneeling or stair climbing
Signs of possible meniscus injury?
- Common symptoms one may report:
- Delayed effusion (6-24 hours post-injury) is a common complaint due to inflammation.
- Feeling a “pop” while trying to abruptly change directions with or without contact
- Twisting injury, such as changing directions
- Reports of “clicking”, “catching” or “locking”
- You don’t necessarily need to have pain or symptoms to have an injured meniscus!
Medical Imaging Tests:
- Magnetic Resonance Imaging (MRI): Useful to diagnose soft tissues injuries, but not all cases may the injury be detected or the actual source of one’s pain. Getting examined to assess your clinical presentation may be more beneficial in helping you recover from your injury.
Examinations a Physical Therapist may complete:
- If the tear is acute, there are a cluster of signs/ symptoms a physical therapist may help determine the likelihood of injury.
- 5/5 symptoms (below) present: 92.3 % positive meniscus injury; 75% likelihood with 3/5 (Lowery et. al 2006)
- History of catching or locking
- McMurray Maneuver- positive may be a pain or audible click
- Pain with forced hyperextension
- Pain with maximal knee flexion
- Medial or lateral joint line tenderness
*** I just obtained an MRI and my doctor stated my meniscus looks fine. Does that mean I didn’t injure my meniscus? ***
ANSWER: Not necessarily, it is important to realize an MRI may not catch everything. Some individuals may have a degenerative meniscus injury and not have symptoms. It is important to correlate your clinical presentation first instead of relying heavily on imaging.
Deciding whether to have surgery
- Your meniscus has some blood supply in given portions and receives nourishment through various neurovascular structures, synovial diffusion, and mechanical motions. If possible, the ultimate goal is to preserve the cartilage to maintain the health and integrity of your knee.
- Conservative (non-operative): Physical Therapy- Stay tuned for Part II
- Surgical
- No success with conservative measures: meniscectomy, debridement, repair, or allograft transplantation may be completed.
- Meniscus Repair/ Partial Meniscectomy: The goal is to save as much of the meniscus as possible to preserve the joint and prevent early onset of osteoarthritis.
- Complex or degenerative meniscus injury, > 45 years: Possible meniscectomy
- Meniscus injury in outer zone, < 35 years: Possible meniscus repair to preserve as much of the meniscus
- Recovery will vary: Meniscus repair (at minimum 12 weeks) –OR– Meniscectomy (4-8 weeks)
- Did you know! Studies have found completing a meniscectomy results in an increase in contact stress in the knee joint. What does this mean? The significant increased load on the knee may contribute to accelerated cartilage damage and degeneration —> Knee Osteoarthritis down the road.
Should surgery be my first option?
No, no, no. If possible, you should consider conservative measures to maintain your knee health in the long run.
If you are experiencing continuous locking, instability of the knee and significant swelling, surgery may be your only option. In that case, I strongly recommend completing physical therapy to improve your strength for a greater outcome. Remember, surgery can increase your long term risk of knee osteoarthritis because various areas of your knee joint will have to withstand pressures. Thus, you should give yourself the best possibility to have a happy knee in the future!
CITATION
Logerstedt DS, Scalzitti DA, Bennell KL et al. Knee Pain and Mobility Impairments: Meniscal and Articular Cartilage Lesions Revision. 2018. J Ortho Sports Phys Ther. 48: 2, A1- A50.
Lowery DJ, et. al. A Clinical Composite Score Accurately Detects Meniscal Pathology. 2006. Arthroscopy. 22:11: 1174-9.
Snoeker B., Bakker E., Kegel C., & Lucas C. Risk Factors for Meniscal Tears: A Systematic Review Including Meta- analysis. 2013. J Ortho Sports Phys Ther. 43: 6, 352-367.
Photo: https://physioworks.com.au/injuries-conditions-1/knee-meniscus-injury
Alaba adeshigbin
18 Mar 2019Good , informative, other option to think about before delving to surgery